an innovative technique for increasing KG around implants
The periodontium, the supporting structure of the teeth is composed of four elements; the cementum, the alveolar bone, the periodontal ligament and the gingiva. Each of them has a distinct location, composition, architecture and function. The whole system support teeth during function and give the teeth the ability to withstand forces upon different masticatory movements. Periodontal disease is an inflammatory disease of the periodontium which leads to destruction of the structures comprising the periodontium. (Chung et al , 2006)
The maintenance of periodontal health
is related to the presence of adequate zone of keratinized tissue, one of the
two types of oral mucosa;
masticatory mucosa which is formed of a keratinized squamous epithelial cells
over layer of connective tissue (lamina propria) that is firmly attached to the
bone through periosteum. it has less elastic fibers and more collagen tissue,
it is found in the attached gingiva and hard palate. On the other hand, the
lining mucosa is formed of non-keratinized squamous cells epithelium above
layer of connective tissue which contains a lot of elastic fibers, the sub
mucosa is attached to the periosteum and the muscles which makes it movable so
that it could be adapted to the muscles movements. (Listgarten et al , 1991)
As mentioned before the amount of Keratinized gingiva
surrounds the neck of teeth is of great importance for the health of
periodontal apparatus, this amount is measured from the mucogingival junction
to the free gingival margin. Without the
aforementioned type of masticatory mucosa, the liability of periodontal disease
increase with high score bleeding index and plaque index. as periodontal
disease progress , teeth turned to be in un restorable state and get indicated
for extraction (Lang & Löe, 1972).
 |
| amount of thick KG around teeth |
Osseointegrated endosseous titanium
implants have shown a great success in replacing the missing teeth as it became
the first line of treatment for edentulous areas. It was first presented in
1978 by Branemark, the idea of dental implants depended on osseointegration
between the implant surface and the bone, osseointegration is defined as
"direct structural and functional connection between ordered, living bone
and the surface of a load carrying implant. Nowadays, osseoinegration is not
the ultimate challenge especially after the huge development in implant macro
and micro designs. However, long term success and prognosis of the
osseointegrated implants depends to a great extent on the health of the
surrounding soft tissues (Kim et al., 2009 ; Albrektsson, 2010
; Abraham, 2014) .
Implants are more susceptible to the development of inflammation and subsequent bone loss in the presence of plaque accumulation and bacterial infiltration due to several factors (Lin, 2013).
In contrast many authors emphasis the importance of keratinized mucosa in order to achieve accepted success rate, many researches reports that a minimum 2 mm of keratinized gingiva are needed in order to achieve healthy gingiva around dental implants However, no any articles had proved the superiority of non-keratinized gingiva to the keratinized gingiva for any reason. (Lang & Löe, 1972 ; Bouri et al , 2008)

no KG around implant result in severe tissue loss
Keratinized gingiva around dental
implants are necessary to achieve esthetic appearance in the anterior teeth,
also it is more resistant to abrasion, recession, less in plaque accumulation
and inflammation, and easy to manipulate during stage two surgery and
impression making in prosthetic stage. For the aforementioned reasons over
year’s authors have developed many techniques to increase the amount of
keratinized gingiva around the dental implants (Adell et al., 1986)
such techniques are apically and laterally
repositioned flaps , free gingival grafts, acellular dermal matrix allograft ,
coronally repositioned flap and sub epithelial connective tissue flaps (Reddy et al , 2013).
The apical repositioned flap has shown
to predictably increase the width of keratinized tissue around natural teeth.
The increasing height of attached gingiva occurs because of an apical
alteration of the mucogingival junction. Which includes apical displacement of
the muscular insertions. (Reddy et al., 2013)
Although the many advantages of
apically repositioned flap procedure as it is well documented that this
procedure increase the width of keratinized tissue by 3.5mm and minimal
post-operative bone loss. It still has the disadvantage of being unsuitable for
a thin biotype gingival tissue, also the use of sutures to close the flap would
produce tension and displace the flap coronally around the implant healing
abutment making a problem in controlling the desired positioning of the
gingival margin. (Reddy et al., 2013)
Regarding the free gingival graft and
sub epithelial connective tissue graft respectively, they are replied to cases
where there is a shallow oral vestibule; a free gingival graft involves
grafting a donor piece of gingiva to a recipient site. For sub epithelial soft
tissue graft technique, refers to submerging gingival connective tissue under a
partial thickness flap. The gingival connective tissue will induce the
formation of keratinized gingiva. However; these methods have the disadvantage
of having a second surgical site and not being an easy procedure to perform by
general practitioners. (Chung et al., 2006; Huh et al., 2013 ; Elkhaweldi et al , 2015)
Acellular
dermal matrix allograft increases the width of peri-implant keratinized mucosa.
It does not require an additional wound in the recipient site, and its supply
is not limited by the amount of donor tissue. Also the esthetic results of
acellular dermal matrix might be better but the problem associated with the
acellular dermal matrix allograft was relapse or shrinkage. The shrinkage rate at 6
months in a tooth-bearing area using acellular dermal matrix graft was 71%.
(Wei et al 2003) (Jun-Beom Park,2006)
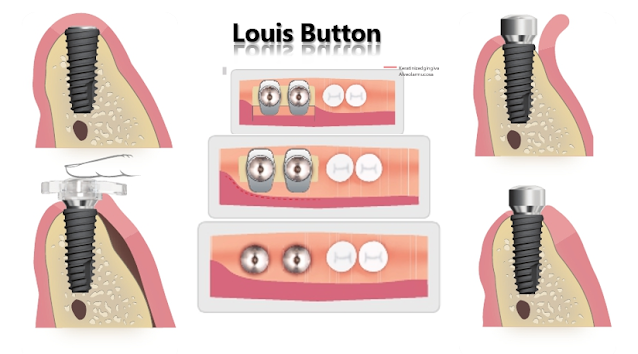
To overcome these problems many investigators have
devised methods for moving the keratinized gingival flap from the lingual to
the buccal and apical directions by fixing a ready-made plastic stent to the healing
abutment.
The stent is made from polypropylene. The buccal
and lingual wings pressing down the flap is 2mm and1mm in size, respectively. The insertion
part of the stent has a cylindrical form (diameter: 4.8 mm, height: 2 mm) that
could hold the healing abutment by friction between the stent and healing
abutment.
. Conclusions:
The use of a
readymade plastic stent in combined full partial thickness apically
repositioned flap shows to be effective in increasing the width of KM compared
to the conventional technique with substantially reduced time and effort.
clinical cases
6 months follow up 9 months follow up
CASE 2 :
- - Ahmed Hamdy, Hala K. Abd El Gaber, Dalia M. Ghalwash, Waleed M. Abbas, "Effect of Using a Plastic Stent with Apically Repositioned Flap in Peri-Implant Soft Tissue Augmentation: A Randomized Controlled Clinical Trial", International Journal of Dentistry, vol. 2021, Article ID 5590400, 6 pages, 2021. https://doi.org/10.1155/2021/5590400






























Comments
Post a Comment